My Approach to Shoulder Pain
A native of San Antonio, Dr. Hinchey completed his medical school and residency training at the University of Texas Health Science Center at San Antonio. He then completed a fellowship year specializing in Shoulder and Elbow Injury and Reconstruction in San Antonio and at the Mayo Clinic in Rochester, MN. Dr. Hinchey practices General Orthopaedics, specializing in all Shoulder and Elbow conditions, treating patients from adolescence to adulthood.
SHOULDER PAIN IS A COMMON AILMENT AMONGST THE POPULATION, WITH INCIDENCE INCREASING AS WE AGE.
Despite technological advances over the past multiple decades, the most important part of determining the cause of a patient’s shoulder pain remains the history and physical examination. In my practice, advanced imaging is typically only used to help support the diagnosis I have formed based on a patient’s evaluation.
ONE OF THE FIRST THINGS I LOOK AT IS THE AGE OF THE PATIENT.
This is important as we can start to form an educated differential diagnosis based on age.
I LIKE TO KNOW THE HANDEDNESS OF THE PATIENT, AND WHAT TYPE OF JOB AND/OR HOBBIES THEY DO. This helps me understand how their ailment affects their day to day activities.
I INQUIRE ABOUT HOW AND WHEN THEIR SHOULDER PAIN BEGAN —was it due to a traumatic event or was it an insidious onset?
ANOTHER MAJOR THING TO KNOW IS, HOW DOES IT AFFECT THEIR SLEEP PATTERNS. In my practice, I have found most patients can tolerate pain until it affects their sleep. Interference with sleep is one of the top reasons patients consider surgical management.
I ASK IF IT INHIBITS THEIR MOTION OR FUNCTIONALITY—for example does it affect lifting items into a cabinet, putting their clothes on, or brushing their hair.
Finally, WE DISCUSS PRIOR TREATMENTS WHICH HAVE HELPED OR NOT HELPED. These include prior therapy programs, medications, injections or possibly prior surgical interventions.
FROM THE MOMENT A PATIENT STEPS INTO THE OFFICE THE PHYSICAL EXAMINATION BEGINS.
When they walk into the exam room, I notice their posture, gait, arm cadence, and overall appearance.
While they are describing their issue, I am watching how they move their cervical spine—is it stiff? Do they guard? Do they hike up their shoulder?
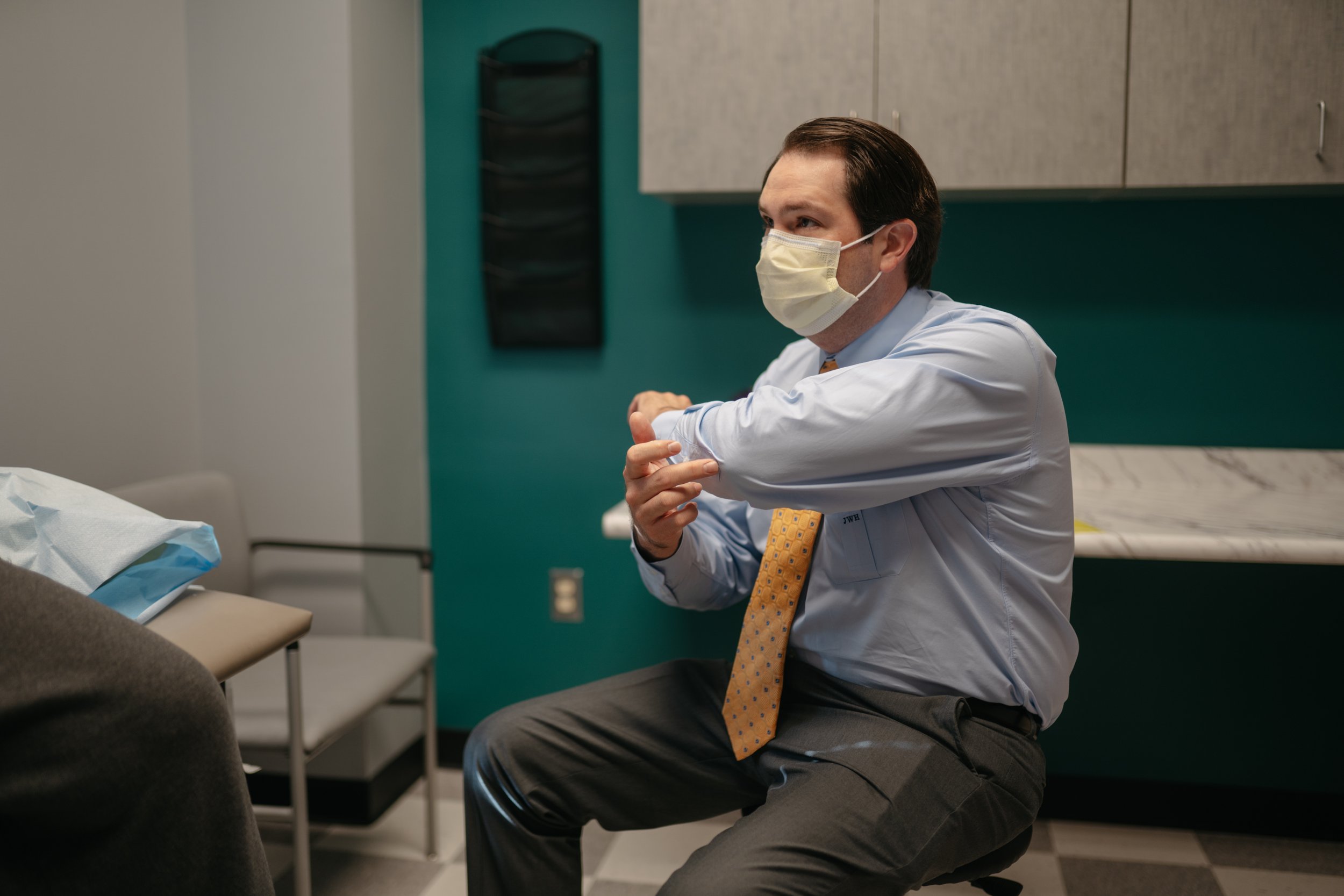
Once we have discussed their issue and how it affects them, I typically move the patient to the exam table and I sit next to them.
THIS IS WHEN THEY BELIEVE THE PHYSICAL EXAMINATION COMMENCES.
I start with observation and palpation of their shoulder girdle and cervical spine. I look for prior scars, rashes, deformities, and feel for areas of tenderness, specifically the acromioclavicular joint which is a very common cause of shoulder pain. We then move on the range of motion, both passive and active, and compare this to the contralateral side. This allows me to assess how their motion differs from the opposite side, and how it affects their function due to lack of mobility. Next, I move on to strength assessment, specific functional muscle and biceps provocative testing, and possibly instability maneuvers. A general overview of the neurovascular status of their affected extremity is also performed, and more detailed assessment if needed.
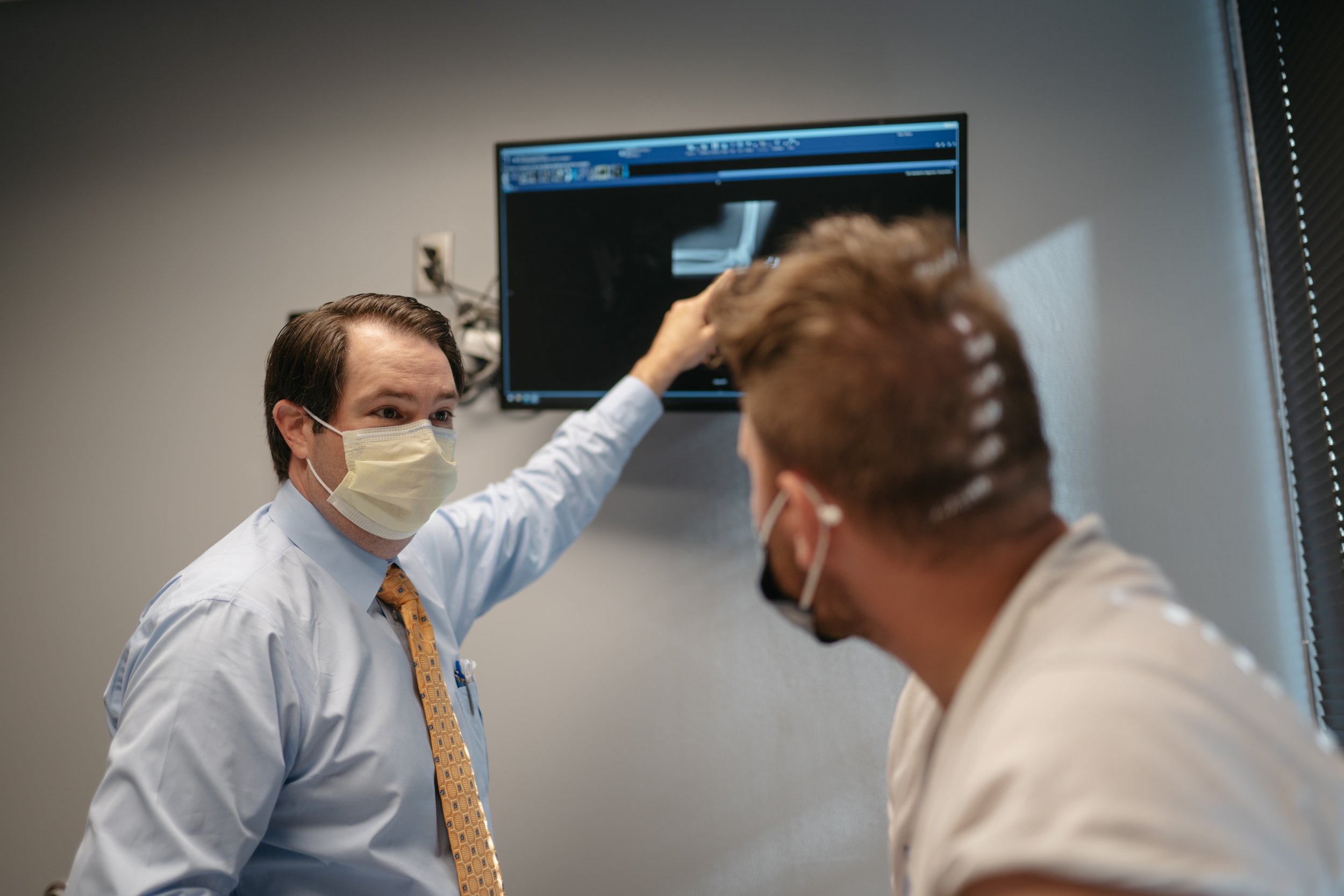
THEN, AND ONLY THEN, DO WE REVIEW THEIR RADIOGRAPHS.
Plain radiographs are still an excellent tool despite the advancement in imaging modalities. From a shoulder radiograph, I can assess for alignment, arthritis, subtle instability, impingement signs, bony erosions and deformity, chronic signs of rotator cuff disease, and, of course, fracture.
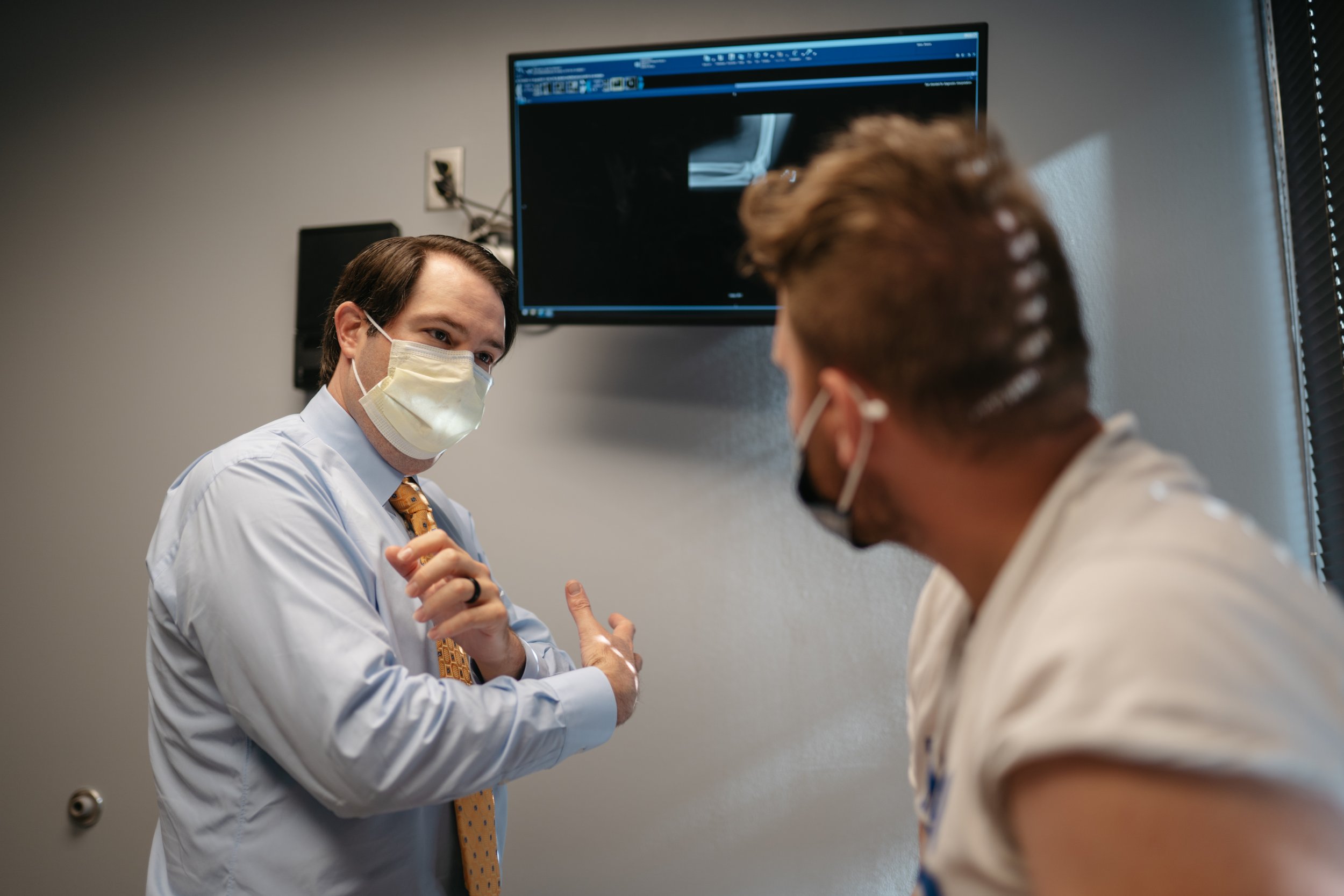
IF ADVANCED IMAGING IS AVAILABLE, AT THIS TIME IT IS REVIEWED. If it is not available, this is when I discuss my differential diagnosis with the patient and if I feel we should obtain advanced imaging or delay it at this time. This all depends on what I feel is their main issue and if it will affect how we treat their ailment.
Finally, a treatment plan is reviewed and discussed with the patient, and their questions answered. I attempt to utilize multiple modalities to help explain what I feel is causing their pain. I use 3d models, education packets, pictures, and demonstrations as much as possible.
The history and physical examination is the cornerstone of medicine, and this still holds true today. In my practice, I take pride in the ability to evaluate a patient and help them in their time of need.